
Mallet Finger Injury
Mallet finger is a common tendon injury that occurs in everyday life. If left untreated, the extensor tendon will not reattach itself to form a permanent deformity.

Mallet finger is a common tendon injury that occurs in everyday life. If left untreated, the extensor tendon will not reattach itself to form a permanent deformity.
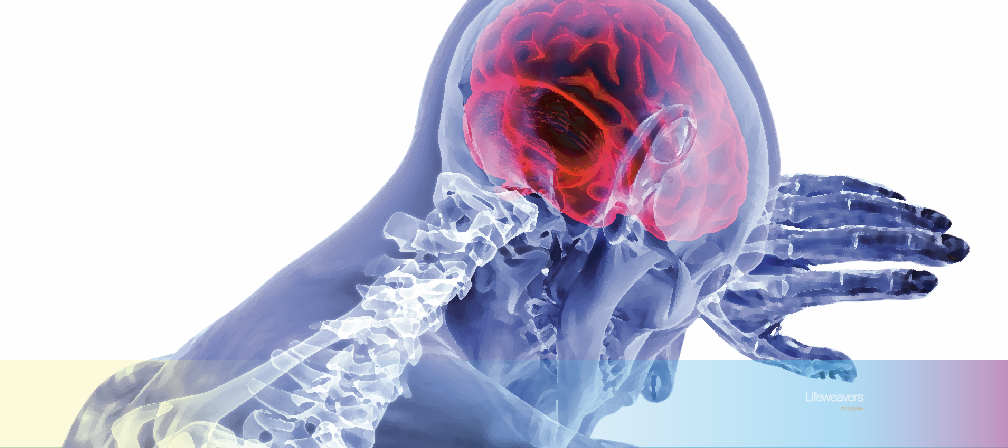
Act as soon as possible after a stroke to maximise the golden window of recovery. The early stage is not a time to rest but for intensive treatment.

In this article, we explore the need for professional therapy and how it impacts one’s life. Is therapy really necessary, you asked?

Shoulder pain is the result of common caregiving mistakes. Why is it serious and how to avoid it. We give 5 simple steps in this article to all the caregivers out there.

Lifeweavers.org explains Social Prescribing, one of the many creative tools our therapy team uses to get people integrating into their communities quickly again.